The healthcare industry is going through a digital transformation with advanced technologies in healthcare applications. Every application has a law standard through which they get approved before reaching out to the customer. It impacts patients’ experience by proving the best apps have the potential to change care delivery by improving patient accessibility and convenience. This blog provides a thorough reference of the essential laws and regulations that govern the Laws for Medical Software Development, allowing you to create apps that are both innovative and compliant.
Additionally, Doctors also prefer apps that fulfil all the Laws for Medical Software Development and security standards. However, this fascinating platform comes with a fundamental responsibility: to ensure patient safety and data privacy. To successfully traverse this complex arena, medical software engineers must have a deep understanding of the regulatory context.
Table of Contents
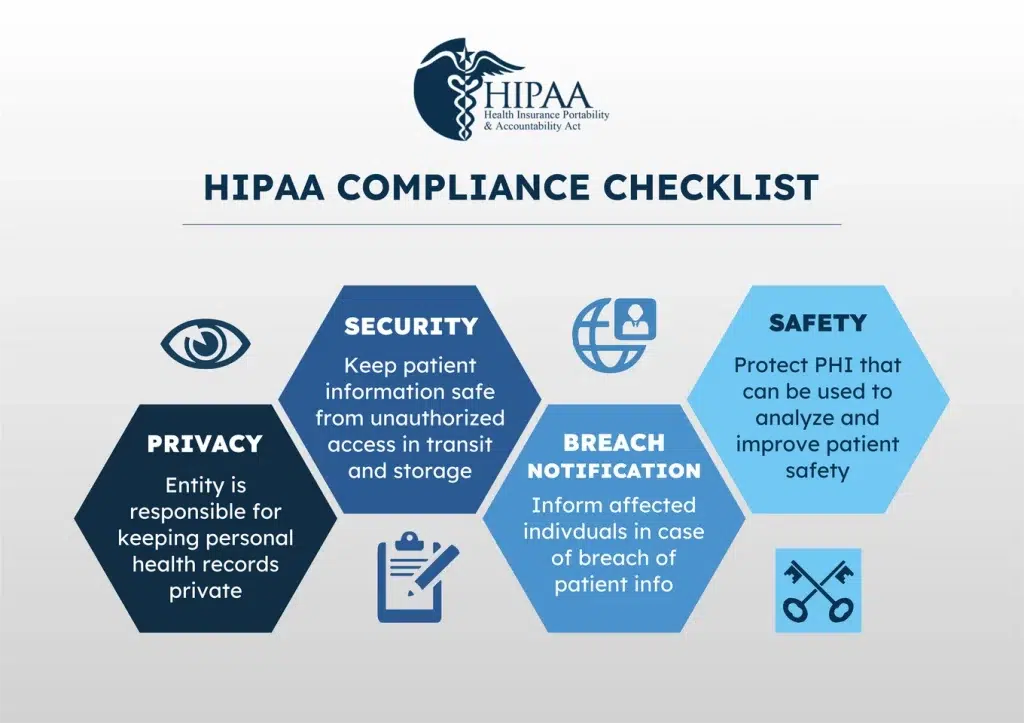
ToggleThe Significance of HIPAA Compliance for Healthcare Application Development Providers
HIPAA, short for the Health Insurance Portability and Accountability Act, establishes guidelines for safeguarding individuals’ private health information. For app developers, not complying with HIPAA regulations can result in significant penalties and harm your professional standing.
To ensure your app is HIPAA-compliant:
- Conduct a risk analysis to identify any vulnerabilities in your system that could compromise patient data.
- Encrypt any personal health information stored on your servers or transmitted between your app and servers.
- Limit access to PHI. Only allow authorized users to access, use, and disclose personal health information. Implement strict login processes for users and track who accesses what data.
- Provide patients control over their data. Empower them to access their health information, make corrections, request restrictions on disclosures, and easily revoke access to their data whenever they choose.
- Ensure proper training. Anyone who interacts with patient data must have appropriate HIPAA training to understand their responsibilities. This includes developers, healthcare providers, support staff, and anyone else with access.
- Have a contingency plan. Establish procedures to identify, respond to, and mitigate breaches of unsecured personal health information. This could include notifying patients and authorities if a data breach occurs.
By making HIPAA compliance a priority in your healthcare app development process, you’ll build an app patients and providers can trust. The time you put in upfront will give you peace of mind that you’re protecting people’s most sensitive data.
The Role of FHIR and HL7 Data Exchange Standards in Building Healthcare Applications
FHIR and HL7 are two of the important standards and regulations guiding the healthcare industry. They establish how health data should be exchanged and shared.
FHIR (Fast Healthcare Interoperability Resources) is the latest standard created by HL7, an international health informatics organization. FHIR makes it easier for healthcare systems and applications to share data by providing a standardized way to format it.
- FHIR resources represent granular clinical concepts like patients, practitioners, medications, etc. These resources can be combined to share complex health records.
- FHIR uses web standards like JSON and XML, so it’s easy for developers to work with.
- FHIR enables seamless data sharing across institutions, platforms, and applications. This helps provide patients with a complete view of their health data.
HL7 refers to a broader set of standards, including FHIR, focused on the exchange, integration, sharing, and retrieval of electronic health information. HL7 standards aim to ensure the meaning, context, and detail of health data transfers are preserved.
By adopting FHIR / HL7 standards, healthcare organizations and technology companies enable more efficient, accurate, and secure data sharing. Patients benefit from improved care coordination and access to their records. Developers gain a framework for building interoperable solutions. And the healthcare system achieves greater productivity, reduced costs, and better outcomes overall.
Emerging Data Standards in Healthcare: ICD-10, XDS/XDS-I, and EVV
Along with the key laws for medical software development in the USA, there are several emerging data standards as well. Compliance with these ensures that your healthcare apps are future-ready for any regulatory changes.
ICD-10
The ICD-10 is a global health data standard for recording and reporting various aspects of diseases, including their causes, symptoms, and social circumstances. Software must be able to generate, store, process, and report this data
- ICD-10 includes approximately 70,000 codes, compared to about 14,000 codes in the prior version (ICD-9). This provides more detailed information about patients’ medical conditions and treatment procedures.
- ICD-10 allows for greater specificity in describing diseases, injuries, and procedures. It improves accuracy in identifying health trends, public health issues, and healthcare costs.
- ICD-10 codes are required for medical claims, public health reporting, and other healthcare data analysis.
XDS and XDS-I
Cross-Enterprise Document Sharing (XDS) and XDS for Imaging (XDS-I) are standards developed to enable the sharing of electronic health records between healthcare organizations.
- XDS defines how to share documents like discharge summaries, imaging reports, and lab results across healthcare enterprises.
- XDS-I extends XDS to share medical images. By using a standardized format to share images and associated data, physicians have immediate access to prior exams and reports, even if they were performed at another facility.
- To build applications supporting these standards, you must understand specifications like ebXML, ebRIM, and DICOM.
Electronic Visit Verification (EVV)
EVV systems use technology like interactive voice response, telephones, and mobile devices to electronically verify home or community-based visits.
As per the Laws for Medical Software Development, medical billing software must have EVV regulations and standards. EVV helps ensure accurate reporting and verification of services delivered. It also prevents fraud by confirming the caregiver’s identity, the recipient, the date/time of service, and the type of service provided.
The Impact of Data Standards on Healthcare Interoperability
Data standards in healthcare aim to improve interoperability between systems and enhance the exchange of health information. When systems can “talk” to each other, providers have a more complete view of a patient’s health history and conditions, leading to better care coordination and outcomes.
Interoperability through Standards
Several standards have been developed to enable seamless data exchange in healthcare. Some of the major standards include:
- HL7 (Health Level Seven International): Focuses on the exchange, integration, sharing, and retrieval of electronic health information. HL7 standards are the most widely used in healthcare IT.
- FHIR (Fast Healthcare Interoperability Resources): Built on HL7 standards, FHIR aims to facilitate health information exchange through an easy-to-implement set of standards. FHIR allows systems to quickly and efficiently share data.
- DICOM (Digital Imaging and Communications in Medicine): The global standard for transmitting, storing, retrieving, printing, and displaying medical imaging information. DICOM enables the integration of medical imaging devices and workstations.
- LOINC (Logical Observation Identifiers Names and Codes): Provides universal codes and names for laboratory tests and other health measurements. LOINC enables the exchange and pooling of results for clinical care, outcomes management, and research.
Driving Efficiency and Improved Care
When healthcare organizations adopt interoperability standards, the benefits are substantial. Providers can access comprehensive patient health data to make the best treatment decisions. Patients receive higher quality, better-coordinated care with fewer errors and duplicated tests. Healthcare systems become more efficient, reducing costs through decreased paperwork, improved care transitions, and the automation of manual processes.
Interoperability powered by standards is transforming healthcare for the better. Although adoption is still ongoing, the future is bright for a fully connected healthcare ecosystem centred around the patient.
Implementing Data Standards in Healthcare Applications
To build effective healthcare applications, you need to understand and implement key data standards. These standards enable seamless data sharing across systems and platforms.
Integrating HL7 Standards
The Health Level Seven International (HL7) organization publishes standards for exchanging, integrating, sharing, and retrieving electronic health information. HL7’s Fast Healthcare Interoperability Resources (FHIR) standard defines data elements and an API for exchanging healthcare information electronically.
Integrating FHIR
When approaching Healthcare Software Development Services, integrating the FHIR standard allows you to:
- Share patient data between providers, payers, and patients
- Enable third-party app integration
- Reduce redundant data entry
- Improve care coordination and patient outcomes
To use FHIR, you’ll need to:
- Choose which FHIR resources, like Patient or Observation, you want to implement based on your app’s needs.
- Expose an FHIR API endpoint in your app that allows Create, Read, Update, and Delete (CRUD) operations on resources.
- Validate request and response data against the FHIR specification.
- Consider security standards like OAuth2 to authorize access to patient data.
Other standards
There are additional standards to consider:
- ICD: The International Classification of Diseases defines diagnosis codes.
- SNOMED CT: A comprehensive clinical terminology used in EHRs.
- LOINC: The Logical Observation Identifiers Names and Codes standard provides universal codes for laboratory and clinical observations.
- RxNorm: Normalizes medication names and dose forms across systems.
Implementing data standards in your healthcare applications will make data more portable and interoperable, allowing for improved care and outcomes. Staying up to date with new releases of standards is key to building innovative, patient-centered software.
Conclusion
HIPAA compliance is vitally important for developing healthcare applications. Noncompliance not only carries serious penalties, but it also damages professional reputation. HIPAA compliance requires thorough risk analysis, encryption of personal health data, restricted access, patient data control, extensive training, and breach response strategies. Furthermore, adopting standards such as FHIR, HL7, ICD-10, XDS/XDS-I, and EVV promotes future readiness and interoperability, resulting in smooth data interchange and better care coordination. Partnering with DreamSoft4u, a seasoned healthcare software developer, gives you access to knowledge in compliance, encryption, FHIR, HL7, and new standards, allowing you to create healthcare solutions that are high in quality, innovative, and compliant.
FAQs
Q1: Which legal considerations should be prioritized when creating healthcare applications?
Prioritizing data security is important for healthcare apps through HIPAA compliance regulation. Additionally, Compliance with FDA rules may also be required for medical devices considering Laws for Medical Software Development.
Q2 Are there restrictions governing the creation of healthcare apps in different regions?
The government policies and rules for healthcare apps vary from country to country. Although there is no such restriction, healthcare apps must prioritize the policies of that particular region. For example, in the European Union, the General Data Protection Regulation (GDPR) oversees data protection and privacy, whereas in the United States, HIPAA laws are critical for healthcare app development.
Q3: What are the implications of failing to comply with healthcare regulations during app development?
Noncompliance can result in legal penalties, fines, reputational damage, and even criminal prosecution in severe circumstances. Additionally, breaches in patient data privacy can cause significant financial and reputational harm to healthcare institutions and app developers.
Q4: How can developers verify that healthcare apps comply with applicable rules and regulations?
Developers should perform extensive studies on applicable rules and hire experts who specialize in healthcare law. When you hire healthcare app developer they have exact ideas about implementing strong data encryption and security measures and update their apps regularly to ensure compliance with evolving regulations.
Q5 What are some recommended practices for ensuring compliance throughout the lifetime of healthcare app development?
Best practices include documenting all stages of development and compliance activities, performing frequent security audits and risk assessments, offering comprehensive user training on data protection and privacy, and maintaining up-to-speed on current laws and regulations.



















